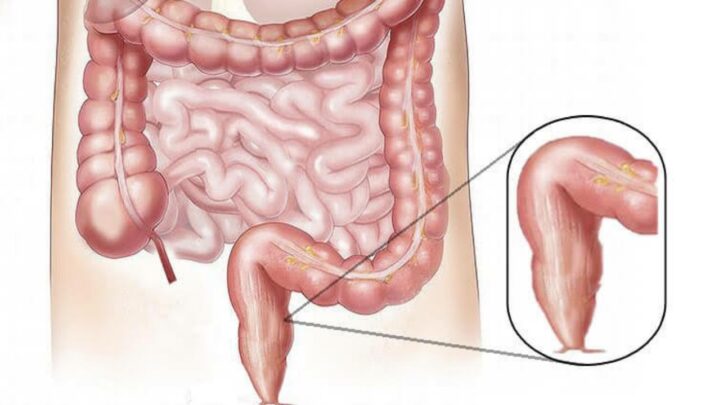
Cancer that starts in the rectum is referred to as rectal cancer. The last few inches of the large intestine are called the rectum. It begins at the end of your colon’s final section and finishes at the short, tight canal leading to the anus. “Colorectal cancer” refers to cancers of the rectum (rectal cancer) and colon (colon cancer).
In many ways, rectal and colon cancers are identical, yet their therapies are vastly different. This is due to the fact that the rectum occupies a small space, barely distinguishable from other organs and structures. Rectal cancer surgery can be difficult due to the limited space.
Even with comprehensive treatment, long-term survival for persons with rectal cancer was once unusual. Rectal cancer survival rates have improved dramatically in recent decades as a result of therapy improvements.
The following are some of the signs and symptoms of rectal cancer:
• Diarrhea, constipation, or more frequent bowel motions are all signs of a change in bowel habits.
• Blood in the stool (dark maroon or bright red) Narrow stool
• Feeling as if your bowels aren’t totally empty
• Pain in the abdomen
• Weight reduction that is unexplained
• Weakness or exhaustion
Causes
Rectal cancer develops when the DNA of healthy cells in the rectum undergoes mutations. The DNA of a cell includes the instructions that tell it what to do.
The alterations tell the cells to grow out of control and to live even when healthy cells would die. A tumour can arise as a result of the accumulated cells. Cancer cells can grow large enough to penetrate and destroy healthy tissue nearby over time. Cancerous cells can also break off and spread to other places of the body (metastasize).
It’s unclear what causes the mutations that cause rectal cancer to occur in most cases. Gene mutations that enhance the risk of colon and rectal cancer are inherited.
Gene mutations passed down from parents to children can raise the risk of colorectal cancer in some families. Only a small percentage of rectal tumours contain these mutations. Colorectal cancer genes raise the likelihood of developing the disease, but they do not make it inevitable.
There are two well-known hereditary colorectal cancer syndromes:
• Lynch syndrome, also known as HNPCC (hereditary nonpolyposis colorectal cancer), raises the risk of colon cancer and other cancers. Lynch syndrome patients are more likely to get colon cancer before the age of 50.
• Familial adenomatous polyposis (FAP) is an uncommon condition that results in hundreds of polyps in the lining of your colon and rectum. People with untreated FAP have a much higher chance of acquiring colon or rectal cancer before they reach the age of 40.
These and additional, less common inherited colorectal cancer syndromes can be detected by genetic testing. If you’re concerned about a family history of colon cancer, consult your doctor to see if your family history shows you’re at risk for these diseases.
Keep reading successyeti.com